Hip Arthroscopy is a minimally invasive operative procedure which allows the treatment of a range of hip joint conditions. It can be used to treat labral (hip cartilage) tears, local areas of joint surface damage, remove loose bodies and undertake simple treatment of early arthritis conditions.
The procedure is usually performed as a “day case” – admitted the day of surgery and discharged from hospital a few hours after surgery. The procedure is normally performed under a general anaesthetic (GA) and for this reason fasting from food/fluid is required before surgery. You will be notified when to stop eating/drinking. You will need to be picked up from hospital by a relative or friend as you will not be able to drive home.
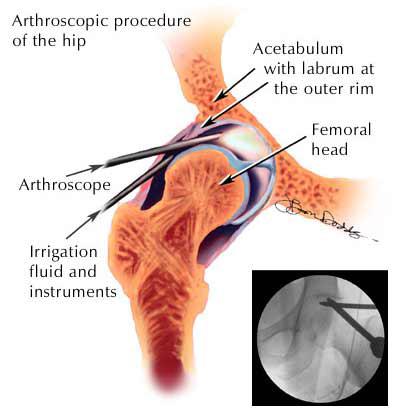
Hip Arthroscopy involves introduction of a small telescope into the hip joint. In order to achieve this the bones of the joint – the ball (femoral head) and socket (pelvic acetabulum) are separated by a small distance. This is done by injecting air and fluid into the hip joint under x-ray control and then applying traction to the foot through a special boot. Two small stab incisions (approximately 5mm in length) are then made over the side of the hip to facilitate firstly the introduction of the joint telescope and then a series of working micro-instruments can be inserted through the second incision. These instruments enable the surgeon to undertake appropriate corrective action relevant to the pathological conditions that may be present.
At the end of the procedure local anaesthetic is normally injected into the hip to minimise pain post operatively and the small incisions are closed with stitches and steristrips. A waterproof dressing is then placed over the area. Your surgeon will normally come and speak with you regarding the procedure before being discharged home. Sometimes the wound will be redressed in the day surgery area before being discharged – particularly if there has been any significant fluid leakage beneath the original dressing.
When you are discharged from hospital you should have a set of photographs from your procedure, some painkillers which will probably be required for a few days, a pair of crutches and a sheet of instructions for your physiotherapist. It is often easier to hire crutches from a local pharmacy or supplier – these are easier to return compared with hospital supplied crutches. Please bring these with you on the day of your surgery. It is not generally recommended to start physiotherapy until after post operative review by your surgeon at 10 – 14 days. If you need a certificate for work/study, please ask your surgeon on the day.
Once you get home it is generally recommended that you mainly rest for the first couple of days. It is normal to feel discomfort and sometimes swelling locally in the groin and thigh. Please use painkillers and ice for this especially in the first 48 hours. Small amounts of bleeding beneath the dressing are very common and not a cause for concern. It is advisable to use crutches to assist with walking and weight bearing activity in the first 5 – 7 days. It is usually okay to put some weight on your operative leg over this period and proceed to full weight bearing after about a week. It is also not advisable to drive in the first 2 – 3 days after surgery. After a couple of quiet days at home you may increase activity slowly as comfort permits. There are no specific exercises to follow at this point – you may move the hip/leg freely provided it is comfortable. Avoid excessive walking, prolonged standing, squatting or deep bending and any significant rotational movements of the leg. Your surgeon will advise you if there are any changes to these basic post-operative guidelines. Should you have any concerns, consult your surgeon or general practitioner.
The post operative visit is usually at 10 – 14 days after surgery. At this time your dressing and stitches will be removed and the surgical wounds inspected. Your surgeon will normally discuss with you the surgical findings and procedure, going over your surgical photographs. At this stage it is normally recommended that you start a hip rehab program under the guidance of a physiotherapist who can tailor the program to your particular condition. Heavy impact activity and sport is usually avoided in the first 6 -8 weeks but gentle low impact activity such as stationary cycling and swimming/hydrotherapy are okay once your surgical wounds are well healed. Rehab usually consists of progressively regaining range of movement of the hip, strengthening exercises to the hip girdle muscles but also to your core muscles (lower abdominals and spine) and some proprioceptive exercises (a combination of balance and coordination work).
As with any operation there are potential risks and complications that can occur. Fortunately these are infrequent and hip arthroscopy is generally regarded as a relatively low risk procedure – however should a significant complication occur you could be worse off than before the procedure. There is a very small risk associated with any form of anaesthesia. Should you have any concerns in this regard, please speak to your anaesthetist who will see you before surgery. There is a small risk of infection developing in the hip and a small risk of deep vein thrombosis (blood clot) developing in the leg – the risks of both are less than 0.5 percent. There is risk of permanent damage to vessel or nerve around the hip – around 1 in 1000 cases. Short lived numbness around the hip, genitals and in the lower leg is slightly more common and if present usually lasts a few days before resolving. Unfortunately there is no procedure (hip arthroscopy included) that fixes all problems and there is a chance that you may continue to experience problems with the hip after surgery of this or any type. Occasionally a hip joint may be very stiff and if the joint cannot be separated satisfactorily, there is a small chance that the surgery will not be able to be undertaken. Despite these potential problems associated with hip arthroscopy, in most cases the surgery results in significant improvements in pain and function.
Recovery following surgery is quite variable and dependant on individual factors, the original hip condition and it’s treatment and your body’s response to exercise / physiotherapy. Your surgeon and physiotherapist should be able to guide you in this regard.