What medications need to be ceased before a surgical procedure?
This is a very common question that crops up before surgery. Medications that increase the possibility of complications such as bleeding or infection or thrombosis ideally need to be ceased prior to undertaking surgical procedures. Frequently these medications are taken for important medical conditions and as such, at times, consultation between your treating surgeon and the prescriber of the medication (GP or physician) will need to take place. This is to devise a plan for how and when the medication should be ceased and whether any covering medication is required and importantly when medication needs to be recommenced after surgery and how this will take place.
Blood Thinning Agents
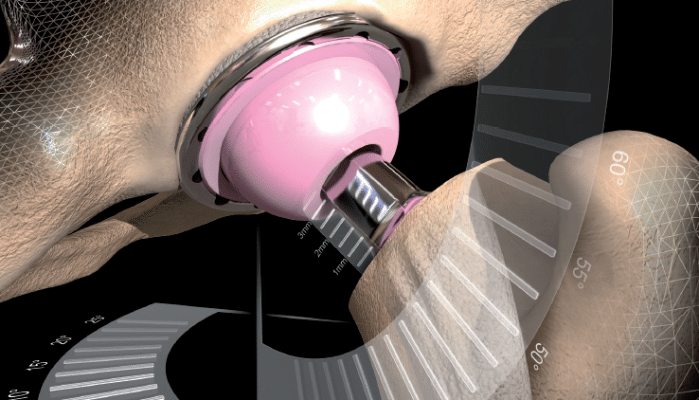
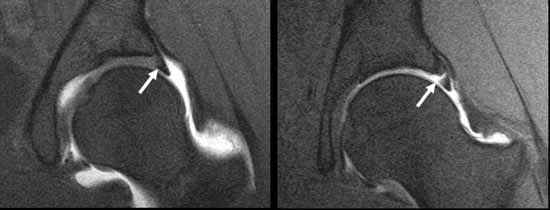
The issue with these drugs is their ability to increase surgical blood loss. This is clearly important in major open cases such as joint replacement surgery, where blood loss can be significant and ongoing loss after surgery can occur if normal clotting mechanisms are impaired. Bleeding can even be a problem in minimally invasive surgery such as arthroscopy. Usually the joint is filled with a clear fluid (normal saline) which provides clear and easy vision to allow the arthroscopic procedure to take place. Bleeding inside the joint (and particularly bleeding that is difficult to control) creates a “tomato soup” effect rather than a clear visual field. If this is bad and can’t be cleared, the procedure may need to be abandoned.
A. Aspirin and Anti-Inflammatory Drugs
Common medications leading to blood thinning include aspirin and non steroidal anti-inflammatory drugs (NSAID). Examples are Astrix, Cardiprin (aspirin) and Voltaren, Naprosyn, Nurofen, Mobic and Celebrex (NSAID). These affect platelets and their function for about a week. It is recommended that these agents are stopped 7 – 10 days before surgery.
B. Platelet Aggregation Inhibitors
More powerful anti-clotting agents like clopidogrel affect platelets also but their effect is longer lasting than for aspirin/NSAIDs and it is recommended that these agents are stopped at least 14 days prior to a surgical procedure. Examples include Plavix and Iscover.
These agents are often prescribed in patients with coronary artery stents in the first 12 months after insertion to prevent stent blockage from occurring. In this time period it is probably better to avoid elective surgery or if surgery needs to be undertaken, advice is sought from the treating cardiologist.
C. Warfarin
Drugs like Warfarin (Coumadin) which effect clotting pathways are usually stopped 5 – 7 days before surgery as this is the sort of time required for clotting to normalize. This can be checked with a simple blood test. Warfarin is often given to prevent stroke in individuals with cardiac arrhythmias such as atrial fibrillation, as a treatment for venous thrombosis and in patients with certain types of artificial cardiac valves. Sometimes in these circumstances Warfarin or similar agents need to be replaced with agents that have a short duration of action (Clexane/Heparin 24 hours) to provide anticoagulation cover until the day before surgery. If the matter is urgent Warfarin can be reversed quickly with VitaminK or infusion of fresh frozen plasma.
D. Oral Heparin-like Agents
Newer agents such as Rivaroxaban and Epixaban are becoming more frequently used instead of Warfarin because of their relatively short duration of effect and the fact that they don’t need to be constantly monitored with regular blood tests. These agents can generally be safely ceased the day before surgery.
E. Glucosamine/Chondroitin
It has been suggested in some studies that Glucosamine and Chondroitin and large doses of Omega-3 oils (fish oil/krill oil) can adversely affect clotting and should be ceased 14 days before surgery.
I’m generally happy for all these agents to be recommenced a couple of days after surgery, provided that ongoing blood loss has ceased and the patient’s condition is medically stable.
Other Medications Affecting Clotting
The oral contraceptive pill (OCP) and hormone replacement therapy (HRT) have been shown to increase clotting and therefore the risk of developing deep vein thrombosis. These agents should be ceased 1 week prior to any surgery where there is a significant risk of deep vein thrombosis – total knee and hip replacement procedures or major pelvic surgery.
Immunosuppressive Medications
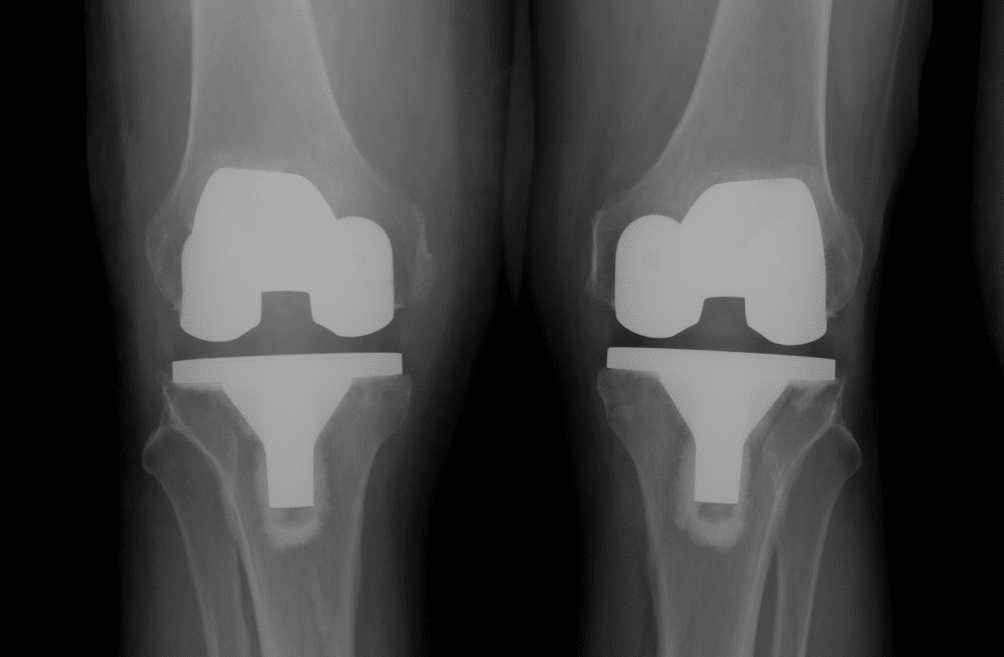
These medications include Methotrexate, Humira, Arava etc and even Prednisolone or Cortisone by mouth and are often prescribed in individuals with auto-immune disorders such as rheumatoid, psoriatic and other inflammatory arthritis conditions. In a surgical setting, these drugs can make the body more susceptible to developing infection and impair the ability to fight infection. These drugs also retard normal skin and soft tissue healing. As such they pose a hazard, particularly in patients undergoing major surgery such as joint replacement procedures. These drugs should be ceased at least one half-life before surgery (usually 1-2 weeks) and should not be recommenced until wound healing has taken place (usually after post operative review at 2 weeks).
Drugs Affecting General Health
Cigarette smoking has been shown to retard bone healing. Smoking also increases anaesthetic risk and risk of developing post operative chest complications such as atelectasis and infection. Ceasing smoking as long as possible before any upcoming surgery will diminish these risks and in situations where bone healing is important (fracture treatment and joint replacement surgery), it is essential that smoking is avoided post operatively. This is common sense anyway in terms of improving general health.
Excessive long term alcohol consumption leads to impaired wound and soft tissue healing. Cessation and vitamin supplementation can reverse these effects in some individuals.
On the Day of Surgery
With surgical procedures scheduled on a morning operating list, patients are requested to fast from midnight. It is generally recommended that usual morning medications are not taken in this circumstance. The anaesthetist may allow some medications to be taken with a sip of water after pre operative anaesthetic consultation. For patients scheduled for surgery in the afternoon, it is generally recommended that usual morning medications are taken at about 0730 with a light breakfast before fasting commences.
For patients with diabetes, every effort is made to schedule these patients early on an operating list to avoid excessive fasting times. For morning list patients, do not take diabetic medications in the morning (oral tablets or insulin). A fingerprick blood glucose measurement is usually undertaken soon after admission to hospital and if low from fasting, glucose via a drip is often started after anaesthetic consult. For afternoon list patients it is recommended that half the normal dose of insulin or medication is taken with an early light breakfast and the same blood glucose measurement process is followed on admission to hospital and adjustments made accordingly.