Inflammatory Arthritis of the Hip, like all forms of arthritis, is due to a loss of the cushioning joint surface tissue (articular cartilage) that covers the ends of the bones of the joint – the femoral head (ball) and the acetabulum of the pelvis (socket). The end result is the same as that of osteoarthritis – with progressive loss of articular cartilage, ultimately leading to a “bone on bone” arthritis situation.
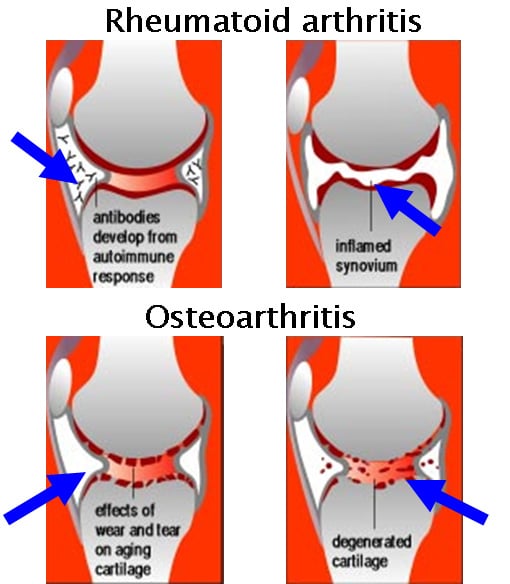
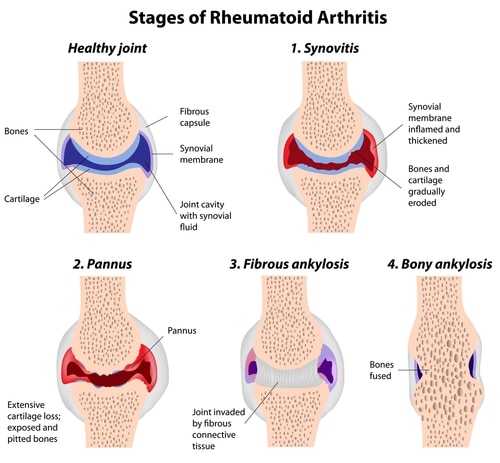
Inflammatory Arthritis differs from Osteoarthritis (OA) in the way that the articular cartilage layer is lost. Inflammatory arthritis frequently has an auto-immune basis – meaning that cells and molecules (antibodies) that would normally protect the body tissues, instead start to attack certain tissues (the synovial lining of the hip) which in turn releases chemical factors that actively “digest” the articular cartilage surfaces of the joint. Using the car tyre analogy – osteoarthritis is tread wear caused by driving thousands of kms, whereas inflammatory arthritis is akin to throwing acid onto the tyre surface which actively eats away the tread.
Conditions associated with inflammatory arthritis of the hip include Rheumatoid Arthritis, Psoriatic Arthritis and Systemic Lupus Erythematosus. Crystal deposition diseases such as gout can lead to arthritis.
Symptomatically inflammatory arthritis of the hip causes the same symptoms as osteoarthritis – pain, stiffness and reduced function for activity/walking. The examination findings also are the same as for OA, but frequently the picture on xray is a little different.

The treatment principles for inflammatory arthritis and OA of the hip are very similar, with conservative measures being appropriate in mild and moderate forms of the disease – namely education, lifestyle and activity modification, weight reduction if appropriate, the use of physical aids and medication with simple analgesics and non steroidal anti-inflammatories being the mainstay. Immunosuppressive or disease modifying medications and corticosteroids can sometimes be helpful, but should only be taken after consultation with and recommendation by a specialist rheumatologist.
Similar to Osteoarthritis, surgery is only indicated for patients with end stage arthritis (bone on bone contact) and unmanageable pain and significantly impaired function. Total Hip Replacement (THR) is the treatment of choice in this situation, as it is generally very successful in providing pain relief and restoring function.
Please read the section on Hip Osteoarthritis – for an overview on hip arthritis.
Source: https://www.parkclinic.com.au/inflammatory-arthritis-of-the-hip/
