What can you reasonably expect in the post operative period following total hip replacement surgery?
After undergoing total hip replacement (THR) surgery it is hoped that you will be able to resume an active lifestyle without the pain of arthritis. This will take time to achieve and you may need to alter the way you perform certain activities in order to protect your new hip and maximize the life of the implant. Unquestionably you will need to be a partner in the healing/rehab process after surgery to obtain the best result possible.
Directly after hip replacement surgery, you will spend some time in the post op recovery area before returning to the ward. There will be a bulky dressing over the wound on the side of the hip and a drain tube or two exiting from the bottom end of this dressing. A special pillow will be sitting under the operated leg, keeping the hip in slightly flexed position whilst maintaining neutral rotation. The ward staff will be checking your observations (pulse, blood pressure, temperature and oxygen saturation) on a regular basis and making sure you are comfortable. Often you will have a handpiece with a button to push for pain relief – patient controlled analgesia (PCA) is a device that allows for small doses of a strong pain-killing medication to be given with each push of the button. You will be encouraged to wriggle your feet and toes to maintain circulation in the legs.
A number of things should happen on the day following surgery. Your surgeon, physiotherapist and specialist physician (if applicable) will visit. In most cases a blood test will be undertaken to check blood levels. An xray of the hip will usually be performed to check the position of the implants. You will start a regime of bed exercises to assist you in moving around in bed, for pressure care and to start movement and muscle function in the operated leg. Sometimes the physiotherapist will stand you out of bed and maybe take a few steps with a frame if you are up to it. The physio will also show you some breathing and coughing exercises to reduce the risk of lung congestion/infection – a common early post-operative problem. You will have antibiotics intravenously in the first 24 hours post surgery and an injection under the skin each day to reduce the risk of thrombosis in the legs. Sometimes special foot pumps are used to prevent clots and anti-embolic compression stockings where appropriate will be applied to the legs.
Figure 1. Day One – up with physio and a walking frame and foot pumps in action when resting in bed.
On the second day after surgery, your blood levels and xrays will be checked by your surgeon. If all is well, most patients have their drains removed (and sometimes IV drip as well) in preparation for starting walking. Your physiotherapist will start this process, showing you the correct way to get in and out of bed and the correct way to walk with a frame. This will usually allow a visit to the bathroom for a shower and toileting. Many patients will sit out in a chair for a period to read or have a meal. Being upright and out of bed assists with pressure care, clot prevention and improves breathing and generally helps you get going. The best defence against complications is to get moving early.
Over the next few days the plan generally is to increase time spent walking and to progress onto crutches. You will be encouraged when safe to go to the bathroom and get out of bed yourself – the staff will let you know when it is OK to do this. You will undertake a program of exercises to get your leg moving which will assist with walking and general mobility. Once you are able to walk a reasonable distance independently, can get dressed and shower without assistance and can negotiate steps and stairs, then you may be in a position to go home. Some people will need a stay of rehab for some more intensive physical therapy before going home. This will be decided on by your surgeon, in consultation with physiotherapist and nursing staff, in accordance with the wishes of the patient. Generally the hospital stay following hip replacement surgery is 5-7 days.
Figure 2. Negotiating stairs with crutches requires technique and practice, but is an essential pre-requisite before discharge home.
On discharge from hospital, you will be supplied with medications (painkillers and sometimes anticoagulant drugs), a set of crutches and an arrangement will be made for your surgical clips/sutures to be removed – usually a nurse will visit but sometimes you may need to attend your GP clinic. A toilet raise and pick-up stick should have been supplied, together with an appropriate chair if required. In most cases it is safe to head home by car (as a passenger not driver), but occasionally an ambulance transport vehicle may be advised.
At home it is expected that you will undertake the same kinds of activities performed in hospital – significant periods of rest punctuated by short bursts of activity. This activity should include walking with crutches (it is recommended that 2 crutches are used strictly at least in the first 4 weeks followed by a period using a single crutch or stick indoors out to 6 weeks) and a specific program of hip girdle strengthening exercises, sometimes with visits to physiotherapy. Some health insurers provide for physiotherapy visits at home. You may make short car trips as a passenger and walks outdoors if you feel comfortable. The aim is to increase walking and exercises progressively each week. You may progress this as much as you feel is comfortable – your body and hip will let you know pretty quickly if you overdo it. If this happens (and it does to most people) you need to rest and just back up a bit with the activity. This will allow you to recover and then push forward again. I can’t stress enough that you need to progress at your own pace and listen to your body – everyone is different and it is sometimes not helpful to pay too much attention to family members, friends and others who have undergone hip replacement who may feel you’re not doing enough or too much. Listen to your body and your physiotherapist will help to guide you. In my experience in the first 6 weeks it doesn’t matter whether you progress quickly or more slowly – this will not affect the end result. Bear in mind that it is going to take at least 6 months and probably closer to 12 months to properly recover.
There are a number of “hip precautions” to be aware of once you have returned home. Largely these involve avoiding certain leg positions to avoid the potential complication of hip dislocation. The risk of hip dislocation is greatest in the first 6 – 8 weeks because soft tissues such as the hip capsule and muscle tendon units that are important for stability have often been violated in undertaking THR surgery. These tissues need 6 – 8 weeks to heal and tighten, providing the new hip with improved stability. These precautions include:
- Sleeping on your back with a simple pillow between your legs – avoiding lying on your side.
- Sitting in a chair which allows your hip to be at a height above the level of your knee. Preferrably the chair should have arms to allow you to ease down and rise comfortable without twisting the hip/leg. Sitting in a low chair without arms puts your new hip in a dangerous position.
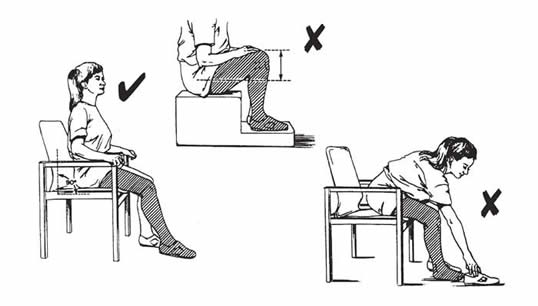
- Avoiding stretching exercises trying to bring your leg up to your chest. Avoid sitting with your legs or knees crossed over. These positions create a risk of dislocation.
- Avoid bending over to pick up objects off the floor or getting into low cupboards. Use a pick up stick or if you must bend down ensure that you are facing the object concerned and place the operated leg a little way behind you maintaining hip extension whilst gently bending the non operated knee. If you are in a sitting position and drop something onto the ground DO NOT bend down to pick it up – stand up first and then proceed as described with pick up stick or a “safe” bending technique.
Figure 4. The safe way to bend down to pick up an object after hip replacement.
Rearrange things in the home so that important objects are in places easy to access. Move furniture, loose electrical cords and rugs so that you have unimpeded walkways and minimize the risk of falling.
You will be sent home with pain killing medication and anti-thrombosis (TED) stockings. Sometimes anti-clotting medication and/or iron supplements are prescribed. A pick-up stick, long shoe horn and sock device can be helpful. Wearing slip on shoes is sensible early.
In most cases a member of the nursing staff will come and visit you at home around 12 days from surgery to remove stitches or surgical clips, inspect your wound and to see how you are getting on. Once stitches have been removed a dressing on the wound is usually not necessary and you may get it wet but dry off well. A moisturizing agent can be applied to the skin if desired. Observe the wound each day – if you develop redness or discharge, notify your doctor. Leg swelling following hip replacement is normal and may take several months to disappear. Elevation, regular icing and using compressive stockings when up and about will help. Should you develop calf pain, chest pain or shortness of breath, contact your surgeon or general practitioner as these may be signs of a blood clot (deep vein thrombosis/pulmonary embolus).
A post operative review is scheduled for the 6 week mark following hip replacement surgery. You should have an xray of the hip just before this appointment to bring on the day. Your surgeon will examine your hip looking at hip movement, muscle strength, balance and the surgical wound. If these parameters and the xrays are OK, then usually you can progress your walking, discarding crutches progressively. Walking is the best overall exercise for your hip and body. Most people need to continue with some specific hip muscle strengthening exercise to assist with balance and endurance for walking. Your surgeon and physio should help guide this process.
After 6 weeks you can generally sleep on your side. Most people will sleep on the non-operated side first and it is recommended that you place a pillow between your legs for a few weeks. It is quite safe to sleep on your operated leg if it is comfortable to do so.
You may recommence driving at this stage if you feel confident. It is important that you are able to get in and out of the drivers side of the car safely. You should practice applying the brake quickly and forcefully as may be required in an emergency situation. If you can do these things then it should be safe to drive a short distance. Don’t plan to drive for long periods initially.
You may also recommence other simple activities at this time (eg. gardening, stationary bike, swimming, light gym exercise etc.) provided you feel comfortable and confident. If you have any doubts about any activity or exercise, then DON’T do it. Sports and past-times like golf, dancing and bowls can be safely commenced after 3 months from surgery. Return to work can be contemplated after 6 weeks if you have an office/sedentary job. If there is a significant physical component to your work then it may take up to 3 months to resume. The aim in the first 6 months is to progress walking, activities of daily living and simple recreations back to a level that you are normally accustomed to. 6 months is the minimum period of time taken to properly recover from hip replacement surgery but remember that most people will take close to 12 months to completely recover. Take your time –recovery is not a race!




